BME in the Center of Washington, D.C.
Letter from the Department Chair

The George Washington University (GW) Department of Biomedical Engineering (BME), located in the heart of Washington, D.C., provides unparalleled access to federal agencies and labs. BME is adjacent to GW’s School of Medicine and Health Sciences and the GW Hospital, which allows for impactful interdisciplinary collaboration with our medical colleagues in our research projects. Our current research efforts include the development of biophotonic tools to advance personalized medicine, new technologies for understanding electrical conduction abnormalities in the heart, developing next-generation biocompatible recording and simulation devices, and engineering novel therapeutic platforms for cancer treatment. In addition to world-class research, our core faculty is committed to teaching our undergraduate and graduate students. We take pride in our small class sizes, nurturing and inclusive environment, and collaborative learning experiences. Finally, all of our core faculty are involved in student-oriented service, including advising, with the goal of equipping our students for a range of career paths from engineers to medical doctors to patent lawyers. Our research, teaching, and service efforts have been recognized by our steady increase in ranking, including climbing six spots in the US News ranking since last year.
Our department is pleased to announce that two outstanding faculty members have joined our community since last Fall. Professor Punit Prakash joined in the Fall of 2024 as the Alisann and Terry Collins Professor of Biomedical Engineering. Prakash’s expertise is in energy-based, image-guided interventions for cancer treatment. Professor Junghun Cho joined us in the Summer of 2025 as an Assistant Professor of Biomedical Engineering. Cho’s research focuses on developing novel quantitative maps of critical brain tissue properties to advance understanding of brain function and neurologic disorders. Finally, our department would like to give our immense gratitude for all of the outstanding contributions of Professor Murray Loew, who retired in the Summer of 2025 after 50 years as a faculty member at GW. We are happy that he will stay on as Professor Emeritus and continue working on his many clinical projects dealing with acquiring and extracting useful information from medical images.
Overall, we are all looking forward to another year of interesting research, teaching, and interactions with students and colleagues!
Vesna Zderic, Ph.D.
Professor and Chair
Department of Biomedical Engineering
School of Engineering and Applied Science
The George Washington University

BRIDGING DISCIPLINES TO ADVANCE ASSISTIVE TECHNOLOGY
Bridging engineering theory with real-world impact, BME students taking the graduate course Rehabilitation Medicine Engineering are co-designing assistive technology alongside students in GW’s Doctor of Occupational Therapy (OTD) program. This collaboration between BME Professor Victor Krauthamer and OTD Professor Kellie Sawyer reflects GW’s culture of interdisciplinary learning, linking technical problem-solving with patient-centered care.
Teams completed a final project based on case studies detailing challenges faced by individuals with physical and cognitive impairments, like “Jolie,” a 7-year-old deaf girl. To help her communicate with those not fluent in sign language, students designed a glove and application that detects and translates the sign language alphabet into on-screen text. Both disciplines valued incorporating each other’s feedback to better understand how the device could improve quality of life.
For OTD candidates, the collaboration showed how reliable technology can enhance care, while their clinical experience helped BME students shift from a purely technical perspective to one grounded in real-world needs. BME students learned the basis of disability, regulatory requirements of medical devices, and testing the end product. Using GW’s Innovation Center, they also prototyped their designs, a key step toward commercialization.
This hands-on project prepares students to communicate across fields and address patient needs, reflecting GW Engineering’s commitment to responsible innovation. The growing partnership offers a model for how interdisciplinary collaboration enhances learning and improves lives.
“MAGNETIC TWEEZER” TECHNOLOGY OFFERS FUTURE OF PRECISE, REMOTE SURGERY
Robots have become increasingly pervasive in fulfilling a host of functions across our society, often to support complex or burdensome tasks. One such task is assisting surgeons in performing surgery with enhanced control and precision, frequently resulting in improved patient outcomes like reduced discomfort and faster recovery.
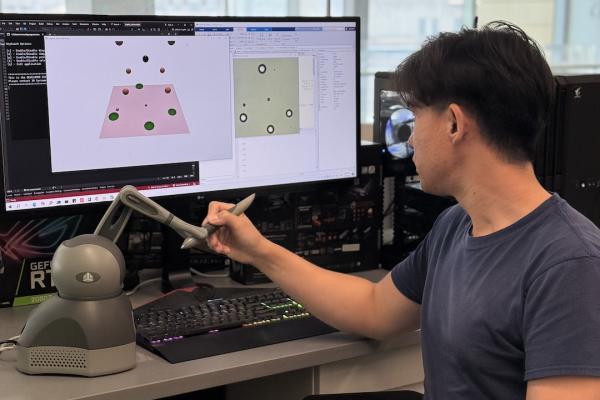
Professor Chung Hyuk Park and collaborators at Southern Methodist University (SMU) have developed a “magnetic tweezer” system that allows doctors to control microrobots, or tiny robots, remotely to conduct non-invasive, precise operations effectively.
Park, the Director of the GW Assistive Robotics and Tele-Medicine (ART-Med) Lab, was approached by a colleague at SMU to join the project because of his expertise in haptic interfaces. Park’s research typically focuses on the collaborative innovation between human intelligence and robotic technology, integrating assistive robotics, machine learning, computer vision, and haptics.
The magnetic tweezer system allows the microrobots to be controlled externally using magnetic fields and offers real-time feedback through a haptic device, similar to a joystick. This device allows the operator to feel forces acting on the microrobots as they move. The magnetic fields, through teleoperation, can work on microrobots more than 1,300 miles away, allowing operators to deliver treatment precisely and minimize risks.
Park’s magnetic tweezers present a new frontier for robotic surgery, easing the burden on surgeons and yielding more promising patient outcomes.

Amy Fehr’s Path to Biomedical Innovation that Puts People First
Amy Fehr, B.S. ‘24, M.S. ‘25, came to GW Engineering inspired by the care her mother received at the GW Hospital for a rare autoimmune condition and stayed because she found a community equally committed to patient-focused innovation. Supported by the Clark Scholars program, she dove into the BME Department’s five-year Bachelor’s/Master’s program, gaining the skills to turn her passion into impact.
The Clark Scholars program provides not only financial support but also a range of experiences that emphasize academic excellence, leadership, and community service. Fehr selected the program’s research track, sharing that it was her peers’ encouragement that led her to pursue and land a research position in Professor Luyao Lu’s lab. As a Dean’s Fellow in her fifth year, she shaped programming for incoming scholars and offered them guidance. For Fehr, this was a full-circle moment as she was able to give back and help others find the success she saw through the program.

Fehr began supporting Lu’s published research on bioresorbable, implantable medical devices in her junior year. In her senior year, she assisted with a project developing an optoelectronic multimodal measurement probe in collaboration with Northwestern University. Her master’s thesis focused on a microfabricated, silver nanowire-based cardiac monitor capable of monitoring heart activity on a tissue level to uncover disease propagation patterns. The nanowire’s flexibility allows it to sit on mobile tissue without causing harm, and its transparency enables fluorescent and electrical mapping. While not yet in clinical use, contributing to such research was deeply meaningful to Fehr.
“I can see this changing somebody’s course along their treatment, just like someone else’s innovation did for my mother,” she said.
Now weighing multiple career paths from medical device design to advanced nanofabrication, Fehr’s education has opened various paths for her to pursue before she returns to academia for her doctoral degree. As she embarks on this new chapter, she carries forward the department’s people- first mindset.
“It’s not just engineering for a salary. It’s engineering for the sake of improving the world.”
Designing Cutting-Edge, Accessible Medical Devices to Diagnose Patients at the Point-of-Care
In healthcare, the accessibility of medical diagnostic devices is critical—not only in emergency situations where minutes, or even seconds, matter, but also in everyday care. Are these devices readily available, and how quickly can they determine the cause of a patient’s ailment?

To answer these pressing questions, Professor Zhenyu Li’s group develops medical technology for personalized medicine and medical research. Li’s passion for making actionable medical information accessible at the point of care has driven his development of multiple microtechnological medical devices, including a microfluidic bioanalyzer using small volume samples such as a drop of blood or tear, and a wearable ECG sensor ring.
There are only a few microliters, or thousandths of milliliters, of tears in your eyes at any given time, making it challenging to analyze tears with typical biological lab equipment. Analyzing tears can help determine how the eye will react to certain stimuli, like contact lenses, and help practitioners make recommendations to help the patient avoid discomfort or infection.
Li, in collaboration with the Food and Drug Administration (FDA) and Johnson & Johnson, has developed a microfluidic device to test human tears with contact lens material. The device helps determine which contact lens material will minimize the patient’s discomfort and identify which contact lens solutions would best suit the patient.

GW’s unique nanofabrication and imaging center allows Li and his team to prototype and test devices right in the Science and Engineering Hall, giving them the unique opportunity to refine their designs on-site. Additionally, GW’s close proximity to the FDA headquarters allowed Li and his team to start their initial collaboration. GW’s Office of Innovation and Entrepreneurship helped the team file a joint patent with Johnson & Johnson Vision Care and identify testing opportunities with local companies.
Li’s medical technology research reflects the unique experience of conducting BME research in the center of Washington, D.C. Li’s research engineers cross- disciplinary, impactful solutions to empower the medical field and the public to give and receive the best care possible.

Engineered in DC, Built for the Farm: Students Design for Real-World Needs
Every day, Gary, a 67-year-old Maryland farmer and recent amputee, struggles with chores due to poor circulation, causing his wrist and forearm to feel cold. Determined to make a difference, a team of BME students made Gary’s needs the focus of their senior capstone project. Through months of testing and collaboration with Gary and local partners, they applied their engineering and problem-solving skills to design two custom warming prosthetic devices to help him continue the work he loves.
Gary requested a warming sock for daily use, which students crafted featuring heating pads between sock layers and a compact LiPo battery secured by a sleeve. A thermostat regulates the temperature and turns off the power when 40° C is reached. A significant design oversight was revealed when Gary struggled to put it on one-handed, which team member Luca Caruso, B.S. ‘25, emphasized they could have easily overlooked without direct user feedback.
The warming sock was also integrated into Gary’s Dorrance Hook Prosthetic. In this setup, the warming pads are layered with Proflex and silicone, fully encapsulating the heating system. Four thin Flexcell batteries were used to maintain a lightweight design that conforms to the prosthetic’s curvature, while a simple on/off switch on the outer shell provides a seamless interface.

To customize both devices, the team benefited from access to industry-grade technologies, such as Direct Dimensions’ 3D scanner, which captured data from Gary’s arm. This advanced technology helped them visualize where the battery and heating pads would lie on Gary’s arm and print 3D models used extensively in the design process and for presentations. A second partner, Volunteer for Medical Engineering, hosted events during the academic year, offering feedback and exposure to other capstone projects.
While some students, like Luca Caruso, have continued their education or entered the medical device industry, this experience will serve as a reminder that user-centered design is a necessity in biomedical engineering innovations and showcases how students at GW Engineering can improve lives even before graduation.

Alumna Tiba Alshammari on Leading with Curiosity as a Future Physician
The interdisciplinary nature and clinical relevance of GW’s BME program attract students from across the globe and from a myriad of academic backgrounds, including recent graduate Tiba Alshammari, M.S. ‘25, who joined the M.S. BME program in 2024 from the University of Virginia, where she earned her B.A. in Cognitive Science.
Alshammari shared that she was concerned about entering the program without an engineering background, but quickly noticed how supportive and encouraging her professors and classmates were.
“I’ve learned so much, not only technical skills, but how to think creatively and design thoughtful, evidence- based solutions,” she shared.
Alshammari appreciated how she and her classmates could explore the real-world application of engineering principles in fields like orthopedics, ophthalmology, and endocrinology.
“We were always encouraged to think critically about where engineering and medicine intersect, but also to ask, ‘What’s missing? Who does this affect? How can we make it better?’ This line of thinking and questioning resonated with me, and the project-based structure of my courses pushed me to learn how to read literature, identify gaps, and build something meaningful,” she explained.
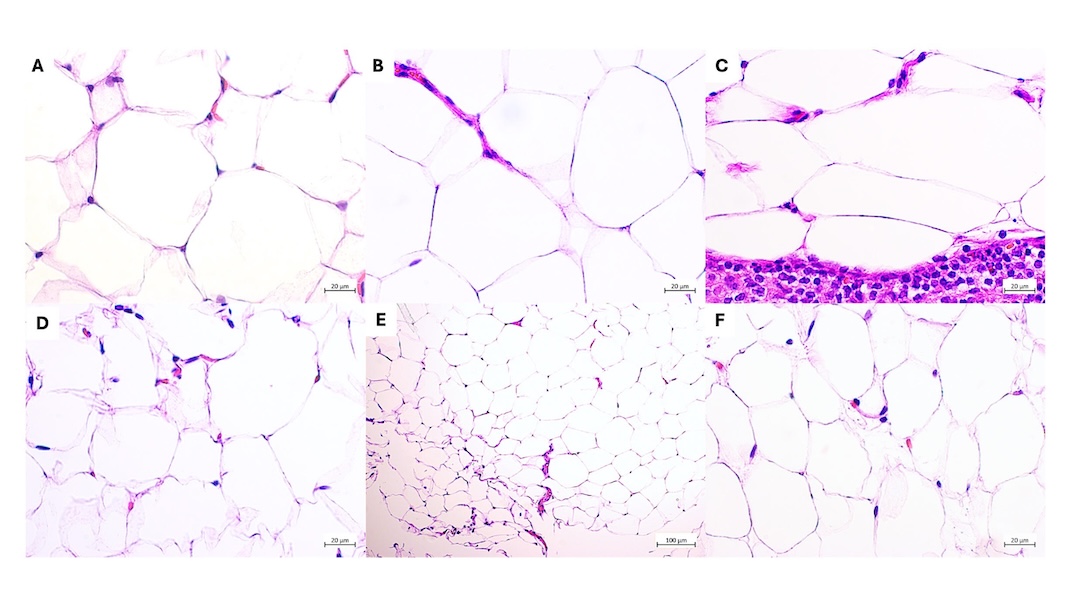
Alshammari completed her thesis under the guidance of Department Chair Dr. Vesna Zderic, exploring how low-intensity ultrasound can noninvasively stimulate the release of adiponectin. Zderic and Alshammari submitted a provisional patent application to protect their novel method and system to stimulate adiponectin release.
Alshammari hopes to see this method further developed and eventually translated into a clinical device that could be used as targeted metabolic therapy, especially for individuals at risk of disease due to obesity.
Alshammari’s experience with the BME department empowered her not only to develop novel solutions to pressing, real-world challenges but also to apply to medical schools. She says her experience with the department shaped how she hopes to approach becoming a physician. “It’s taught me to lead with curiosity, to be innovative, and to always look for deeper understanding in every challenge I face,” she concluded.